If you were to assess 100 people struggling with substance use issues on a given day, it is likely that 99 of them would not be ready or willing to engage in substance use treatment. However, those 99 people would very likely be ready and willing to feel respected, to connect with others who accept them for who and where they are in their personal journeys, and most importantly — to learn how to avoid overdose and stay alive. Harm reduction strategies are a key evidence-based way to prevent death, overdose, and communicable disease, yet the approach is still not widely used — especially in traditional health care settings.
Background on Harm Reduction
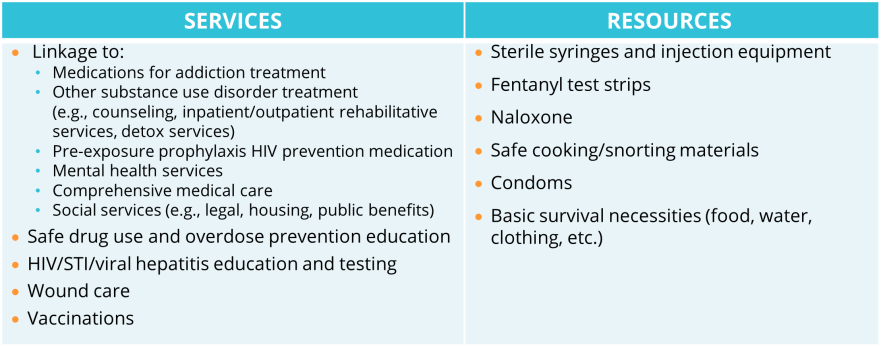
Harm reduction is a set of practical strategies aimed at reducing negative consequences associated with drug use, as well as a movement for social justice built on a belief in, and respect for, the rights of people who use drugs. Harm reduction typically includes a comprehensive range of services and resources (see Table 1). Brick-and-mortar-based harm reduction programs often offer additional services such as access to showers, laundry facilities, and a kitchen.
Table 1. Harm Reduction Services and Resources
While all harm reduction services and resources are valuable, it is harm reduction’s philosophy of radical acceptance and respect for personal autonomy that drives the approach’s effectiveness. Harm reduction settings are non-judgmental spaces where participants are embraced for who they are and “where they are” in their journeys. Harm reduction providers take a “low threshold” approach to offering services with participants supported in identifying their needs and developing their own wellness goals, even if those include the continued use of substances.
While harm reduction has been used for over 40 years in the United States, it has never been more relevant than it is today due to the opioid overdose epidemic and its destructive impact on individuals, families, and communities. Nationally, drug overdose deaths have risen steadily over the past decade with more than 106,000 overdose deaths reported in 2021 — and over 70,000 of those deaths involving synthetic opioids, primarily fentanyl. Fentanyl’s increased presence in the drug supply, which often leads to the unknowing ingestion of fentanyl by people who use drugs, is a primary driver of the increase in overdose deaths. Other synthetic alternatives, e.g., xylazine, are also causing a new range of health issues for people who use drugs.
The Evidence and Missed Opportunity of Harm Reduction
New users of harm reduction services are five times more likely to enter drug treatment and three times more likely to stop using drugs than those who do not use the services. Harm reduction services are also associated with an estimated 50 percent reduction in HIV and hepatitis C incidence. When combined with medications for addiction treatment/medications for opioid use disorder (MAT/MOUD), hepatitis C and HIV transmission is reduced by over two-thirds. While technically forms of treatment, MAT/MOUD are also widely considered forms of harm reduction.
Yet, despite harm reduction’s efficacy in preventing overdoses and the spread of communicable disease, as well as linking people to substance use treatment and other critical health services, the approach has not been more widely adopted. Why? Harm reduction has historically been stigmatized, due to pervasive misperceptions on its impact on people and communities. Evidence shows, however, that harm reduction programs do not enable increased drug use, drive increased crime, or contribute to syringe litter.
People who use drugs are often stigmatized by the health care system, leading to a lack of trust in, and comfort with, accessing health care services from traditional providers. Adopting a harm reduction approach offers a unique opportunity to engage people in care who would otherwise not be comfortable doing so. Providers should consider what they can do to fill the significant gap in the substance use care continuum existing between active substance use and engagement in traditional substance use treatment services — particularly for people deemed to be at high risk for overdose via appropriate overdose risk screening. While there have been some early attempts to integrate harm reduction into traditional health care settings, including hospitals, there is still much room for further innovation aimed at better meeting the needs of people who use drugs and ultimately preventing overdoses, communicable disease spread, and death.
Practical Steps for Adopting a Harm Reduction Approach
There are practical steps providers and health systems can take to adopt a harm reduction approach.
- Learn from people with lived experience. Invite persons with lived experience to speak to staff and leadership about their experiences using harm reduction services and how they were different than experiences with traditional services. Understanding their experience will help inform better programs and policymaking.
- Promote leadership and staff buy-in. Educate senior leadership on harm reduction philosophy, its evidence-base, and its value proposition — the potential to save lives, drive increased linkage to substance use treatment, drive improved health outcomes, and decrease costs. Provide educational opportunities on harm reduction for staff at all levels. Help clinical staff understand how adopting a harm reduction approach can assist with engaging patients who are apprehensive to engage. Illustrate for clinical staff how adopting a harm reduction approach can also decrease provider burnout by providing services that are more of a “fit” for patients and will be met with less resistance.
- Address stigma. Stigma toward people who use drugs is pervasive in our culture, including providers. Engage in education and training to understand and address stigma among staff. It is critical for providers to understand their own biases that may impact how they treat and communicate with patients and provide care.
- Assess the local, state, and organizational policy landscape. Substance use stigma has made its way into law and policy at many levels — particularly with respect to the distribution of syringes. Develop an understanding of existing parameters around the provision of harm reduction services and identify services that are currently permissible to offer. Identify financing mechanisms to sustainably support harm reduction efforts.
- Identify opportunities to engage in policy reform efforts. Providers have an important role to play in harm reduction expansion efforts given their direct service work with people who use drugs, as well as their understanding of how current substance use services often fall short of meeting the needs of the people they serve.
- Develop a collaborative relationship with existing harm reduction providers. Integrating harm reduction services into a traditional health care setting can take time. Until integrated harm reduction services are in place, providers at traditional settings should develop collaborative relationships with local harm reduction providers to facilitate warm referrals for patients who can benefit from services.
- Take an incremental approach. Provide “basic” harm reduction resources at the beginning of harm reduction integration efforts to get staff familiar with the approach. For example, distribution of naloxone and fentanyl test strips can serve as early, basic resource offerings. Find creative ways to promote access to resources among the local community of people who use drugs. Seek out technical assistance opportunities to support phased-in harm reduction implementation.
- Inventory current services provided. Assess the current suite of services provided and determine what can be adopted as part of a comprehensive harm reduction services approach. Many care settings offer HIV, STI, and communicable disease testing — all of which are important parts of broader harm reduction services.
- Assess opportunities to provide Medications for Addiction Treatment (MAT)/ Medication for Opioid Use Disorder (MOUD). MAT/MOUD have emerged as highly effective treatments for substance and opioid use disorder and are also considered a form of harm reduction. Providers should consider opportunities to offer MAT/MOUD if not currently doing so. For providers currently offering MAT/MOUD, there may be opportunities to build on those efforts and have MAT/MOUD serve as the foundation of a comprehensive harm reduction approach. The recent removal of the federal “X-Waiver” requirement has opened the door to more widespread adoption of MAT/MOUD.
- Join local/regional/statewide efforts. Given the severity of the opioid overdose epidemic, coalitions have increasingly been formed to develop coordinated strategies to prevent overdoses and better meet the needs of people who use drugs. Health systems and providers can benefit from joining such coalitions to learn more about the needs of the people and communities they serve and play a role in broader epidemic response efforts.
Connection Saves Lives
“The opposite of addiction is not sobriety, it is connection,” noted the writer Johann Hari, who spent years researching addiction through the perspectives of people on all sides of the issue. Harm reduction opens the possibility of connection for people who use drugs and have otherwise been ostracized by their families, friends, the health care establishment, and society at-large. Through that connection, and harm reduction’s radical acceptance of people regardless of the choices they make, there is the possibility to save lives, drive improved health outcomes among people who use drugs, and begin to turn the tide on the national overdose epidemic.