Headline
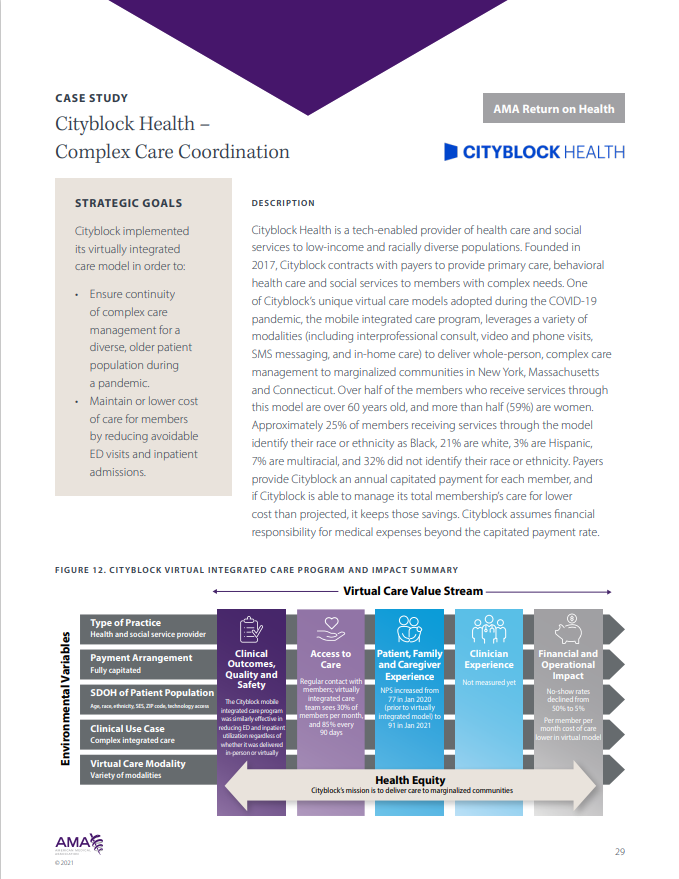
During the COVID-19 pandemic, Cityblock Health implemented a virtually integrated care management model to maintain continuity of care for patients with complex needs.
Context
Cityblock Health provides primary and behavioral health care and social services to populations with complex needs on behalf of payers. This case study details how during the COVID-19 pandemic, Cityblock Health implemented a mobile integrated care program using a mix of telehealth services to maintain whole-person, complex care management for members from communities that have been marginalized. The mobile integrated care team include a community health partner, nurse care manager, nurse practitioner or primary care physician, behavioral health therapist, and psychiatrist. To support older adult members who experienced difficulty connecting for virtual clinical visits, emergency medical technicians (EMT) operated as in-home extenders and initiated video calls, collected vitals and labs, and conducted physical exams during virtual clinical visits.
Findings
The mobile integrated care program was able to maintain continuity of care, seeing about 85 percent of total members every 90 days. The virtual care program cost less than in-person care on a per member per month basis and was similarly effective to in-person care management in reducing emergency department and in-person utilization. When EMTs were sent to homes to initiate and help conduct video visits, no-show rates declined from 50 percent to five percent.
Takeaways
This case study on Cityblock Health’s implementation of an innovative mobile integrated care management model illustrates how organizations can structure an interdisciplinary integrated care team to support individuals with complex needs receiving virtual care management.