Lauran Hardin, MSN, CNL, FNAP, FAAN, Senior Advisor and Mark Humowiecki, JD, Senior Director, Camden Coalition’s National Center for Complex Health and Social Needs
One of the most important aspects of making the case for complex care is to choose the right measures to demonstrate a program’s impact. In a project supported by The Commonwealth Fund, our team from the National Center for Complex Health and Social Needs interviewed more than 100 leaders of successful complex care programs about how to make the value case for complex care. Most had dealt with unrealistic expectations about the timeframe for achieving a positive financial return on investment (ROI).
To support more realistic goals that reflect the breadth of value created by complex care programs, leaders suggested a comprehensive set of measures for the field that expand the definition of ROI while keeping a solid foundation in traditional measures like cost and utilization. This blog post details their recommendations for selecting measures as part of a strong value case.
Anchoring in Equity
Complex care programs typically serve populations that experience health inequities because of things like systemic discrimination and social risk factors. Documenting the demographics of the populations you serve will allow your program to disaggregate health outcomes by race/ethnicity or other factors to ensure delivery of equitable care and improvements in overall health equity. Baseline demographic data should include: race/ethnicity, gender identity, age, zip code, language, disability status, and economic status.
In addition to demographics, leaders recommend documenting key social drivers of health, such as housing, food security, access to benefits, and access to care, which disproportionately impact communities of color and other marginalized communities. This data can provide strong evidence of ROI to the community.
Finally, consider patient- or staff-reported measures regarding equity to round out the picture of your program’s impact. A recent brief from the Center for Health Care Strategies offers several new measures to consider in addressing equity.
Thinking in Quadrants
Complex care programs have many stakeholders — internal organizational leaders, consumers, payers, community partners, and board members, to name a few. Each of these groups have their own definition of what matters in the value equation. When choosing measures for your program, it's helpful to start with three questions:
- What do your stakeholders or funders really care about?
- What measures do your program directly impact?
- Are you measuring what matters to the population you are serving?
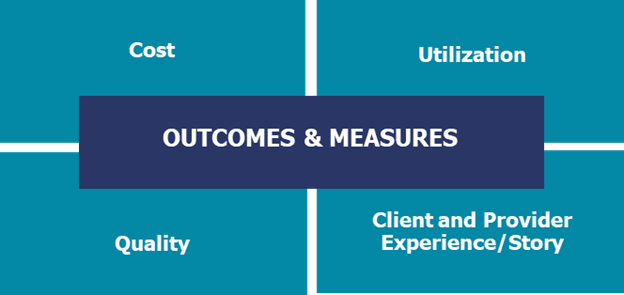
Creating a panel of measures allows you to demonstrate ROI in terms that matter to each stakeholder. A key principle for success is to choose only a few targeted measures in each quadrant that demonstrate your impact. Leaders recommended including measures in each of four key categories — cost, utilization, quality, and client and provider experience.
Cost
Cost is a measure universally used by programs to demonstrate impact, but adding a layer of understanding what costs and for whom can strengthen your case. If your program has a relationship with a payer, you may be able to get total cost of care information from their data. Many programs serve multiple payers and also the uninsured, so finding new ways to represent this data can be helpful. Creating a partnership with health systems can give your complex care program access to hospital and primary care costs.
If this data isn’t available to you, assigning an average cost for an inpatient or emergency department (ED) visit in your market can be a way to demonstrate cost impact. The Kaiser Family Foundation developed a calculator for average inpatient hospital costs per day and Becker’s Hospital Review also publishes average costs per day. Becker’s Hospital Review also publishes average ED visit costs. In our toolkit for building the value case for complex care, you’ll find a tool to estimate your impact on cost with your population.
If you have support from a finance professional and access to data, differentiating your impact on fixed and variable costs can expand the story of your ROI. Variable costs include things like pharmacy costs, length of stay days, or unnecessary testing.
You can also add impact on cost for partnered systems like primary care, behavioral health, and social services. Some programs use EMS transports or the cost of a day in jail depending on the population they serve.
Finally, if your program generates revenue — either through direct billing, gaining insurance for people that results in paid visits, or in increasing appropriate and desired use of care like primary care visits — it's helpful to add that to the value equation.
Utilization
Many complex care programs are focused on impacting utilization, whether that is decreasing unnecessary utilization of the health care system or increasing appropriate use of desired care. Showing your impact in this quadrant is essential. Innovative programs are beginning to add impact on utilization of partner services like an increase in behavioral health visits or a decrease in jail days/recidivism to show community-wide ROI. For example, Adventist Health’s Project Restoration in Clearlake, California impacted EMS response costs and reduced costs from days in jail by coordinating across sectors to meet the needs of their most vulnerable community members.
If you have sophisticated data analytic support, you can add indicators on efficiency in utilization such as impact on length of stay days in the hospital or total minutes of ED visits. These indicators translate into an improved ROI.
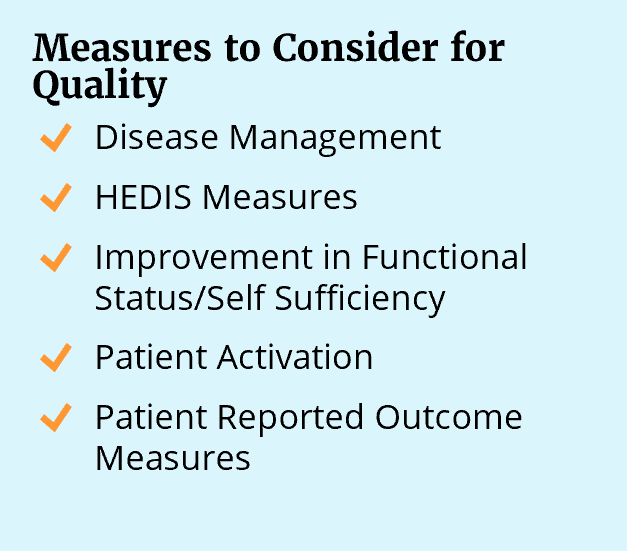
Quality
Choosing a few key measures that show your impact on quality will round out the value equation. If you are impacting disease management, choosing one or two HEDIS measures can be helpful, as they are widely used by payers.
It's helpful to think about measures that demonstrate actual improvement versus the number of people served. Tools like the Arizona Self-Sufficiency Matrix provide an opportunity to assess several domains before and after intervention. The Patient Activation Measure tool is another resource for assessing change.
Finally, thinking about including patient-reported outcomes measures as an indicator of quality is a priority for many. This new resource from the Centers for Medicare & Medicaid and this brief from the National Center for Complex Health and Social Needs offer several recommendations and options.
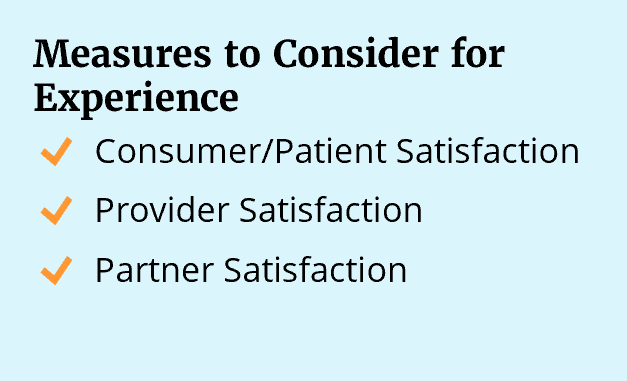
Client and Provider Experience
Evaluating satisfaction is one of the least consistent measures completed by complex care programs but one of the most powerful for demonstrating impact to diverse stakeholders. Creating an avenue for the voice of the consumer to inform program design and demonstrate value and ROI is key. Many programs record patient stories or videos as a baseline. Create opportunities, including surveys or point of care questionnaires, to regularly capture feedback from patients and their family members to add depth to the value equation.
Two other groups that are important to consider include providers and cross sector community partners such as housing services, EMS, and others who intersect with the population. Complex care programs often improve efficiency and reduce complexity for these groups, resulting in job satisfaction and improved delivery — another kind of ROI. Showing how you have impacted provider burnout or partner engagement shows another valuable aspect of complex care intervention.
Demonstrating Impact
Once you’ve identified your measures and collected outcomes, it's critical to share them in a way your stakeholders including internal leaders, consumers, payers and community partners can understand. As part of the Building the Value Case for Complex Care toolkit, the Value Case Summary tool was developed to help programs collect and demonstrate impact in a one-page view.
Translating that information into a visual using infographics will help clearly communicate what you have accomplished. Adventist Health’s Project Restoration Model, for example, created a dashboard of outcomes that is easily shared and understood.
Including a video of a patient story can really drive home the impact from your program. Hearing directly from consumers is one of the most powerful ways for stakeholders to connect to the meaning of the work you are doing. Adventist Health created a video interviewing a consumer and the providers and partners involved in the intervention. In five minutes, they were able to demonstrate the impact directly on consumers but also on the community relationships and network of delivery that is strengthened by the program.
Finally, having a presentation deck ready to show your impact is a helpful tool. The Building the Value Case for Complex Care toolkit includes a draft pitch deck you can adapt to summarize the key aspects and outcomes from your complex care program.
Pooja Bhalla, DNP, RN, Executive Director of Healthcare Services for the Illumination Foundation shared her advice for other programs looking to build a sustainable value case: “My advice would be really, first focus on your care model, what it needs to be for your specific population. Then make sure that you capture the data along the way to tell your story as you're meeting with funders. We work very closely with our marketing team who's constantly producing infographics for us. We can walk into a room with a one-page document they created and show our outcomes and do that elevator pitch pretty quickly. Those things are easier said than done, but I think they go a long way in telling the payer or partner who we are, what we do, and how we do it.”
Taking the time to consider the best measures for your program will set a strong foundation for long-term financial sustainability. Use a foundation in equity and the four quadrants to build a value case that shows ROI not only in dollars, but in life-changing impact on individuals and the community. That’s a real alignment between margin and mission.