By John Findley, MD, Caravan Health Medical Director, ACO Programs
In recent years, the Centers for Medicare and Medicaid Services (CMS) has focused attention on care delivery redesign, most importantly addressing the critical need to increase investment in primary care. While primary care services make up only about 4 to 7 percent of total U.S. health care costs, recent evidence suggests that greater spending on primary care could save a significant amount in downstream costs. Experts have estimated that if primary care spending increased to 12 percent, it could cut both per patient and overall expenditures.
Some of these cost savings would be due simply to better prevention and chronic disease management. Newer clinical programs such as the Annual Wellness Visit (AWV) can elevate the importance of prevention and establish a more comprehensive and patient-centered approach to care. Implementing and building these primary care team capabilities can launch the journey toward value-based care.
The time constraints of the typical primary care practice often do not allow providers to take a comprehensive look at all of their patients’ needs each year. Getting to the bottom of the checklist of preventive screenings and evaluating all ongoing chronic care needs simply takes time. Enabling office staff to assist in this work, under the direction of the supervising provider, presents a tremendous opportunity to create a patient-centered and comprehensive care plan that matches each patient’s unique needs and desires.
The AWV is a Foundational Primary Care Tool
The AWV is an essential instrument in the transition from reactive to proactive care. It is an in-depth medical visit in which the patient and provider share information about health history and concerns, and create a cohesive care plan that they will revisit at subsequent visits. Creating a care plan during the AWV encourages a shift of focus from an acute problem-oriented approach to a more comprehensive and continuous approach. For providers, there is an additional benefit beyond individualized planning for each patient: the AWV helps them understand the health of their patient population.
An AWV every year, for every patient, casts a wide net enabling practices to better understand the population served. It also helps care teams to identify and connect with all providers involved in a patient’s health care journey – establishing the beginnings of better care coordination and a true medical neighborhood.
An established relationship with a primary care provider is a cornerstone of highly effective care coordination. Some patients who come in for an AWV are not yet connected to a primary care physician, making this an opening for that care connection. According to recent literature, less than 10 percent of adults in the United States are receiving all recommended preventive services, with 5 percent receiving none at all.
Researchers at Duke University estimated that in order to conduct all recommended acute, chronic, and preventive care and screenings, each primary care physician with the typical patient load (more than 2000) would have to dedicate more than 21 hours a day. This is clearly unrealistic, and we have to find another solution.
The AWV can lower health care costs through preventive care. A study published in the American Journal of Managed Care of about 9,000 patients in two ACOs showed that those who had an AWV had a 5.7 percent reduction in health care costs in the following year. Notably, the cost savings were greatest for those with more complex, severe conditions based on Hierarchical Condition Category (HCC) score.
Caravan Health Takes a Comprehensive, Nurse-Led Approach to the AWV
Achieving success in population health requires a team. At Caravan Health, we recommend that our partner practices focus on offering AWVs as one of the first steps in transforming care delivery. CMS has recognized its importance as well and offers it as a free annual benefit for Medicare Part B beneficiaries.
How can our practices focus on this time-intensive service when primary care physicians are already overstretched? AWVs can take as long as an hour, depending on the extent of the patient’s health needs. The key to managing this workload is empowering population health nurses. Medicare permits certain non-physician providers to lead AWVs, as long as they are operating under the direct supervision of a physician.
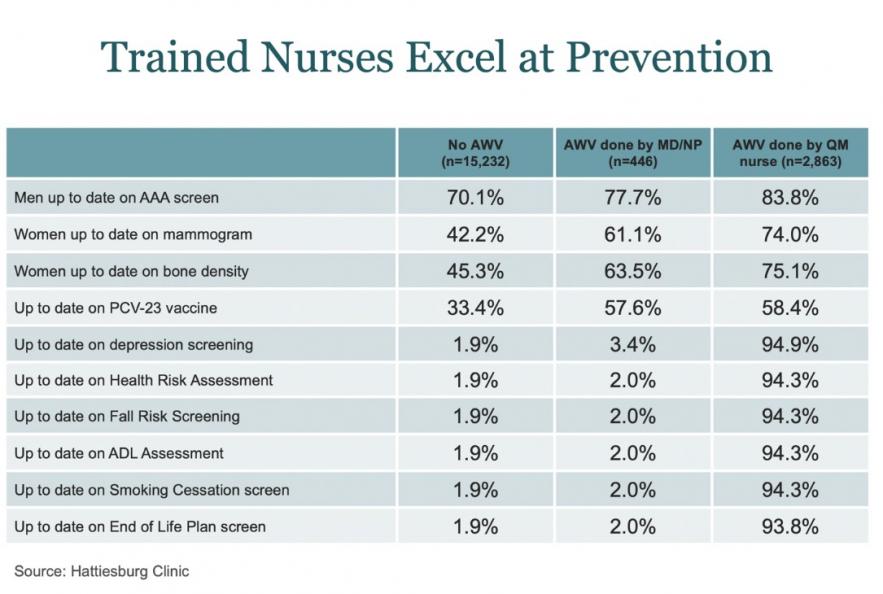
A nurse-led AWV can work well for all involved. With a nurse leading in the delivery of this most needed service, physician time is freed up to oversee and lead care team efforts. The AWV can identify patients in need of higher-intensity outreach efforts and care coordination via the primary care team. This approach ultimately guides future clinical programs efforts such as chronic care management and behavioral health integration. It is also an excellent opportunity to initiate often-overlooked advance care planning discussions as part of a patient-centered care plan. In some clinics, nurse-led AWVs have yielded better outcomes on quality measures than those led by physicians or nurse practitioners alone, as illustrated in this chart.
In Practice — AWVs Help ACOs Excel at Primary Care
To better understand how AWVs can help an individual practice starting out in accountable care, we talked with clinical staff from the North Mississippi Connected Care Alliance, part of a Caravan Health ACO. This provider completed more Medicare AWVs than all of our other partners for three straight years. Brad Crosswhite, the ACO Medical Director, credits this success to a well-thought-out start. “We started this as a small pilot program at one of our clinics and tried to fully leverage the opportunities to make this easy for patients and the providers who perform these examinations,” he said. “Now many of our clinics are performing AWVs on 80-90 percent of Medicare patients.”
Dr. Crosswhite discussed the importance of provider engagement. “I remind our providers that this is not just a checkbox. The AWV is designed to promote value for our patients, to increase care quality while decreasing cost of care. Sometimes it takes repeated one-on-one conversations and group meetings as well. We will use as many avenues as it takes to be sure that we’re really communicating our vision and goal for an ACO.”
Primary Care, Starting With the AWV, Is Central to Value-Based Care
Caravan has consistently seen that taking advantage of this opportunity to spend more time with patients has many invaluable benefits for our partner practices: increased patient satisfaction, improved preventive care, greater ease of quality reporting, and a deeper understanding of the disease burden of the patients served.
CMS has recognized the importance of this valuable work and is willing to pay practices for the time and effort it takes. The AWV creates a clear path toward a financially sustainable future for primary care by generating revenues that can be used to hire additional staff needed to support ongoing population health efforts.